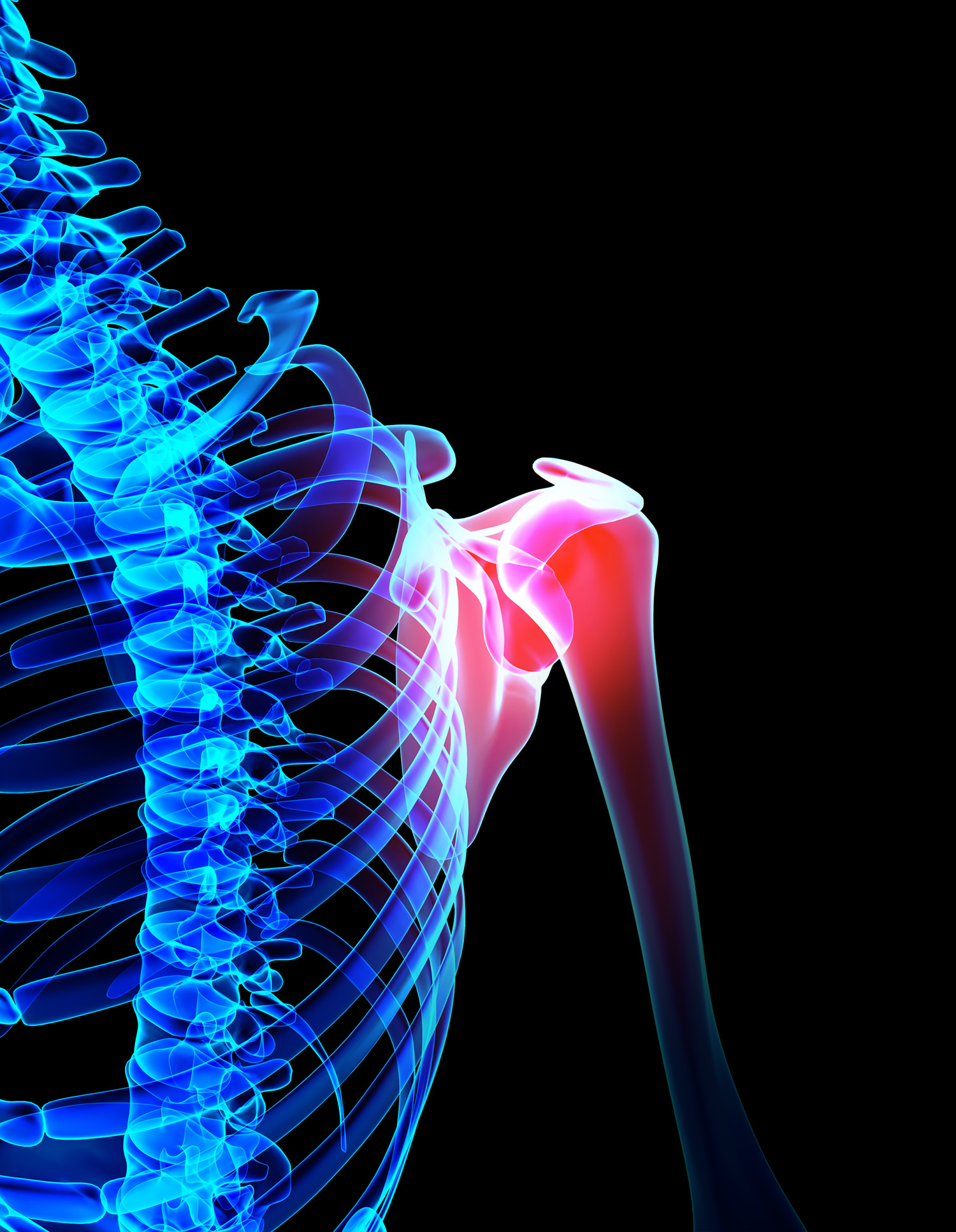
How best to repair the labrum, a cartilage structure that deepens the socket of the shoulder joint, remains somewhat controversial, but knotless sutures and bioabsorbable tissue anchors are some of the technological advances improving outcomes. says orthopedic surgeon Alejandro Badia.
Badia, who is one of the notable hand and upper limb orthopedic surgeons in South Florida, reports significant clinical success in performing minimally invasive, arthroscopic surgery, proving particularly beneficial for closing so-called SLAP tears—injuries to the upper portion of the labrum, the fibrous cartilage that surrounds the rim of the shoulder socket.
The knotless sutures, loaded onto bioabsorbable anchors, are used to reattach the detached labral tissue at the right tension to return the shoulder joint to full movement. Badia says the knotless systems remove the risk of irritating the shoulder joint and also allow for better control of the tension during the repair. The repair of a labral tear/detachment is now done arthroscopically via three small portal incisions, he says.
The labrum helps stabilize the humerus in its socket, whereas the primary role of rotator cuff tendons is to maintain the head within that socket allowing shoulder motion.

Tears in the labrum can be caused by trauma, such as sports-related injuries; repetitive use of the shoulder by athletes and workers for lifting, catching or the overhead throwing of heavy objects; and simple weakening from aging, Badia says.
A common cause of a labral injury occurs when a person instinctively outstretches the arms in an effort to break a fall. Falling directly on the shoulder can also tear the labrum by causing a dislocation of the shoulder joint.
The shoulder is highly vulnerable to disease and injury because it is the most unstable joint in the body, explains Badia, who is founder and medical director of the Badia Hand to Shoulder Center and OrthoNow. “Yet, it is this very instability that provides the shoulder with such an extensive range of motion, allowing it to assume up to 1,000 different positions.”
Patients with labral tears may complain of nonspecific pain and sensitivity in the front of the shoulder, shoulder popping and a general sense of instability in the joint—symptoms that often make diagnosis difficult. Labral tears are hard to prevent as they tend to be from sports-related or traumatic-injury events.
“Shoulder pain is one of the most common musculoskeletal complaints of patients but pinpointing the precise nature of the problem can be challenging and should be done by an orthopedic specialist experienced in treating disorders of the upper limbs,” Badia says.
Labral tears are a common cause of persistent shoulder pain and are difficult to diagnose, even by magnetic resonance imaging. Many times, the diagnosis is made at the time of the arthroscopy, where a fiber optic instrument is inserted into the shoulder, allowing diagnosis and definitive repair during that same outpatient procedure. However, occasional failed labral repairs can be because of ineffective or incorrect suture anchor placement and overtensioning of the labrum tissue and biceps tendon, Badia says.
Badia emphasizes conservative approaches can be initially used with small labral tears including cryotherapy, anti-inflammatory medications, rehabilitation and perhaps injection of certain orthobio agents, such as PRP.
“Surgery should only be performed if rest and rehabilitation are unsuccessful in healing the injury,” he adds. “Any operation should be performed not only to repair the labral tissue but address the injury that resulted in the tear in the first place.”
New mobile transport device can save critical patients
When a patient at a medical facility is so critically ill they would likely not survive a regular ambulance ride to another facility with more advanced life-saving equipment, all is not lost, thanks to a mobile medical transport device available only at Memorial Healthcare Systems.

The device is called a mobile ECMO (extracorporeal membrane oxygenation machine) and is used on only the most critical of patients. Memorial Hospital pulmonologist Lance Cohen, who leads one of the teams when a patient needs this specialized type of transport. “There are two primary utilizations,” Cohen says, adding it can be used for both severely compromised lung and or heart and lung problems.
The ECMO is used to bypass a compromised heart and lungs to keep a patient alive even when their own organs can no longer sustain them. Cohen says ECMO has also been used in cases of severe influenza or pneumonia. Plus, it has also been used in high-risk pregnancies, trauma situations, transplant situations, and auto-immune disorders.
Memorial has two separate ambulances equipped with these devices, Cohen says. One is for adult transport; the other for children. Cohen heads the team of specialists for adult patients. “It’s a highly specialized team,” he says. “We need to practice. It’s like changing tires at a Formula 1 race. We’ve gone as far north as Jupiter, west to Naples and south to Miami-Dade County.
“Not many hospitals have ECMOs. It’s the mobile units that really differentiate us. We can go out and help other centers.”
A new approach to relieving ‘breast implant illness’
Unfortunately, some women who have undergone breast implant surgery complain of a variety of symptoms such as brain fog, joint and back pain, fatigue, hair loss and general feelings of malaise. As a result, a number of these women are opting for breast explant surgery.

One Miami plastic surgeon is using a rather unique approach when removing patients’ breast implants. Physician Joshua Lampert uses a sizer to inflate the breast and then removes a superficial layer of skin. “I’m trying to preserve as much original tissue as possible,” he says. “It’s important to preserve as much as possible.”
Lampert says the sizer enables him to get better counter traction, making it easier to remove the outer layer of tissue.
As to why women might be experiencing these symptoms following implant surgery, doctors are not sure. Lampert says this is called “breast implant illness,” and there is not a lot of scientific evidence available. “We do not know what it is,” he says.
The doctor says scar tissue can be a concern following an implant, and that might be related to the problem. “When scar tissue forms, it causes deformity and pain, and surgery can help.” ♦